Prophylaxis of Surgical Site Infection in Cranial Surgery with Vancomycin Powder Application into Wound
DOI:
https://doi.org/10.36552/pjns.v23i3.351Keywords:
Vancomycin, cranial surgery, surgical site infectionAbstract
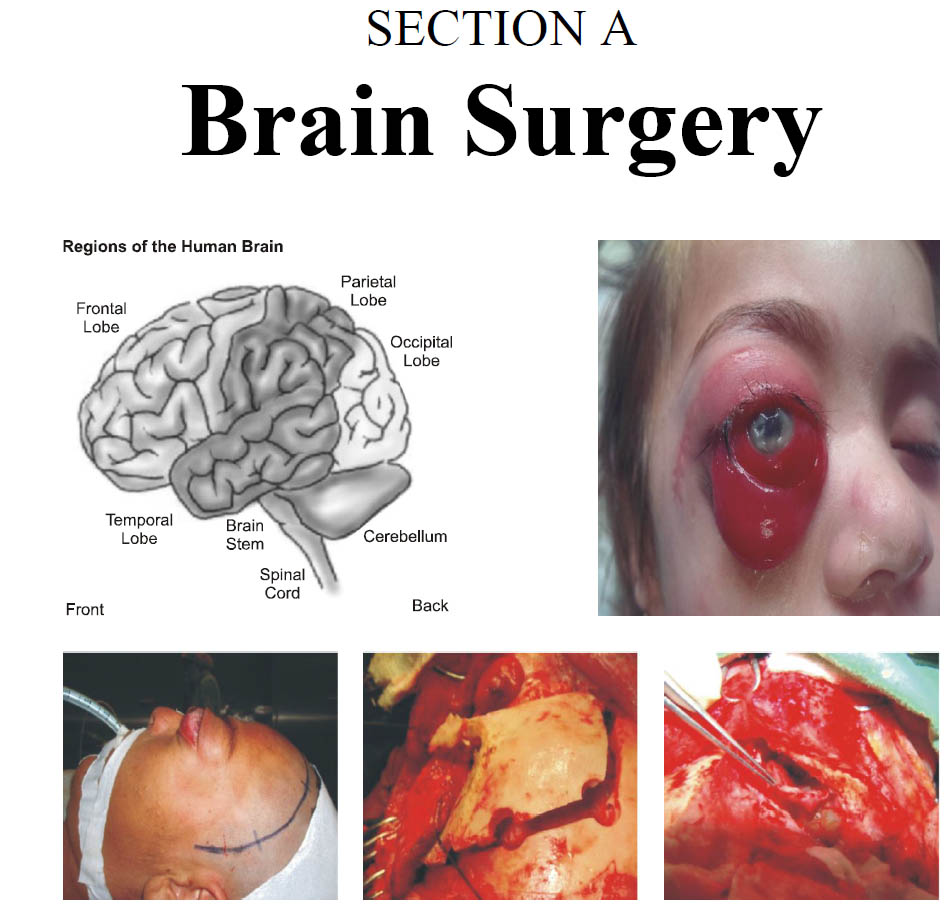
Objective: To see the effect of application of Vancomycin powder directly into the subgaleal space in reducing the postoperative surgical site infections.
Materials and Methods: All the patients who underwent consecutive elective craniotomies from April 2017 to May 2018 Dept of Neurosurgery, szabmu, PIMS, Islamabad. The control group received the standard routine prophylaxis according to the hospital protocols, whereas the treatment group, in addition to the standard prophylaxis, received Vancomycin powder in the surgical wound in addition to the standard routine prophylaxis.
Results: 182 patients were enrolled in the study, 91 allocated to each the control and treatment group (Vancomycin). Six patients were lost to follow up. There were 90 patients in the control group and 86 patients in the treatment (Vancomycin) group. Both the groups were almost statistically similar. In the control group, 34.09% (n = 60) were male and 17.04% (n = 30) were female. In the treatment group, 29.54% (n = 52) were male and 19.31% (n = 34) were female. The overall rate of surgical site infection (SSI) was 3.97% (7 out of 176 cases). A statistically significant difference found in infection rate between the treatment group, 0% (0 out of 86 cases) and the control group, 7.77% (7 out of 90 cases) with the p value of 0.002.
Conclusions: The use of topical Vancomycin powder in surgical wounds may significantly reduce the incidence of infection in patients undergoing elective craniotomies. It is a promising means of preventing devastating and harmful postoperative wound infections.
References
2. Yin CH. Risk factors and outcomes associated with surgical site infections afer craniotomy and craniectomy." University of Iowa; 2012.
3. Chiang HY, Kamath AS, Pottinger JM, Greenlee JD, Howard MA, 3rd, Cavanaugh JE, et al. Risk factors and outcomes associated with surgical site infections after craniotomy or craniectomy. J Neurosurg. 2014; 120 (2): 509-21.
4. Cassir N, De La Rosa S, Melot A, Touta A, Troude L, Loundou A, et al. Risk factors for surgical site infections after neurosurgery: A focus on the postoperative period. Am J Infect. 2015; 43 (12): 1288-1291.
5. Magill SS, Hellinger W, Cohen J, Kay R, Bailey C, Boland B, et al. Prevalence of healthcare-associated infections in acute care hospitals in Jacksonville, Florida. Infect Control Hosp Epidemiol. 2012; 33 (3): 283-91.
6. Walcott BP, Redjal N, Coumans J-VCE. Infection following operations on the central nervous system: deconstructing the myth of the sterile field. Neurosurg Focus, 2012; 33 (5): E8.
7. Fang C, Zhu T, Zhang P, Xia L, Sun C. Risk factors of neurosurgical site infection after craniotomy: A systematic review and meta-analysis. Am J Infect Control, 2017.
8. Buang SS, Haspani MS. Risk factors for neurosurgical site infections after a neurosurgical procedure: a prospective observational study at Hospital Kuala Lumpur. Med J Malaysia, 2012; 67 (4): 393-8.
9. Davies BM, Jones A, Patel HC. Implementation of a care bundle and evaluation of risk factors for surgical site infection in cranial neurosurgery. Clin Neurol Neurosurg. 2016; 144: 121-5.
10. Caroom C, Tullar JM, Benton Jr EG, Jones JR, Chaput CD. Intrawound vancomycin powder reduces surgical site infections in posterior cervical fusion. Spine (Phila Pa, 1976), 2013; 38 (14): 1183-7.
11. Abdullah KG, Attiah MA, Olsen AS, Richardson A, Lucas TH. Reducing surgical site infections following craniotomy: examination of the use of topical vancomycin. J Neurosurg. 2015; 123 (6): 1600-4.
12. Ravikumar V, Ho AL, Pendhakar AV, Sussman ES, Kwong-Hon Chow K, Li G. The Use of Vancomycin Powder for Surgical Prophylaxis FollowingCraniotomy. Neurosurgery, 2017; 80 (5): 754-8.
13. Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control, 2009; 37 (10): 783-805.
14. Mallela AN, Abdullah KG, Brandon C, Richardson AG, Lucas TH. Topical Vancomycin Reduces Surgical-Site Infections After Craniotomy: A Prospective, Controlled Study. Neurosurgery, 2017.
15. Hervin R. Dashti, Humain Baharvahdat, Robert F. Spetzler, Eric Sauvageau, Steven W. Chang, Michael F. Stiefel, et al. Operative intracranial infection following craniotomy. Neurosurg Focus, 2008; 24 (6): E10.
16. O'Keeffe AB, Lawrence T, Bojanic S. Oxford craniotomy infections database: a cost analysis of craniotomy infection. Br J Neurosurg. 2012; 26 (2): 265-9.
17. Kourbeti IS, Jacobs AV, Koslow M, Karabetsos D, Holzman RS. Risk factors associated with postcraniotomy meningitis. Neurosurgery, 2007; 60 (2): 317-26.
18. Proctor LM. The human microbiome project in 2011 and beyond. Cell host & microbe. 2011; 10 (4): 287-91.
19. Shiono Y, Watanabe K, Hosogane N, Tsuji T, Ishii K, Nakamura M, et al. Sterility of posterior elements of the spine in posterior correction surgery. Spine (Phila Pa, 1976), 2012; 37 (6): 523-6.
20. Miller MB, Bassler BL. Quorum sensing in bacteria. Annual Reviews in Microbiology, 2001; 55 (1): 165-99.
Downloads
Published
Issue
Section
License
The work published by PJNS is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Copyrights on any open access article published by Pakistan Journal of Neurological Surgery are retained by the author(s).












