Craniosynostosis: Clinical Presentation and Outcome of Surgical Treatment
DOI:
https://doi.org/10.36552/pjns.v24i3.467Keywords:
Craniosynostosis, strip craniectomyAbstract
Objective: Craniosynostosis presents sclerosis cranial sutures, ossification and fusion involving the vault of the base, sutures involved can be one or more sutures. This study aimed to determine the surgical outcome of craniosynostosis.
Material and Method: The prospective study was conducted at the neuro spinal and cancer care institute, Karachi. Patients presented with sagittal, metopic, unicoronal, lambdoid, bicoronal craniosynostosis were included in the study, while patients with coagulopathy, previously operated cases were excluded from the study.
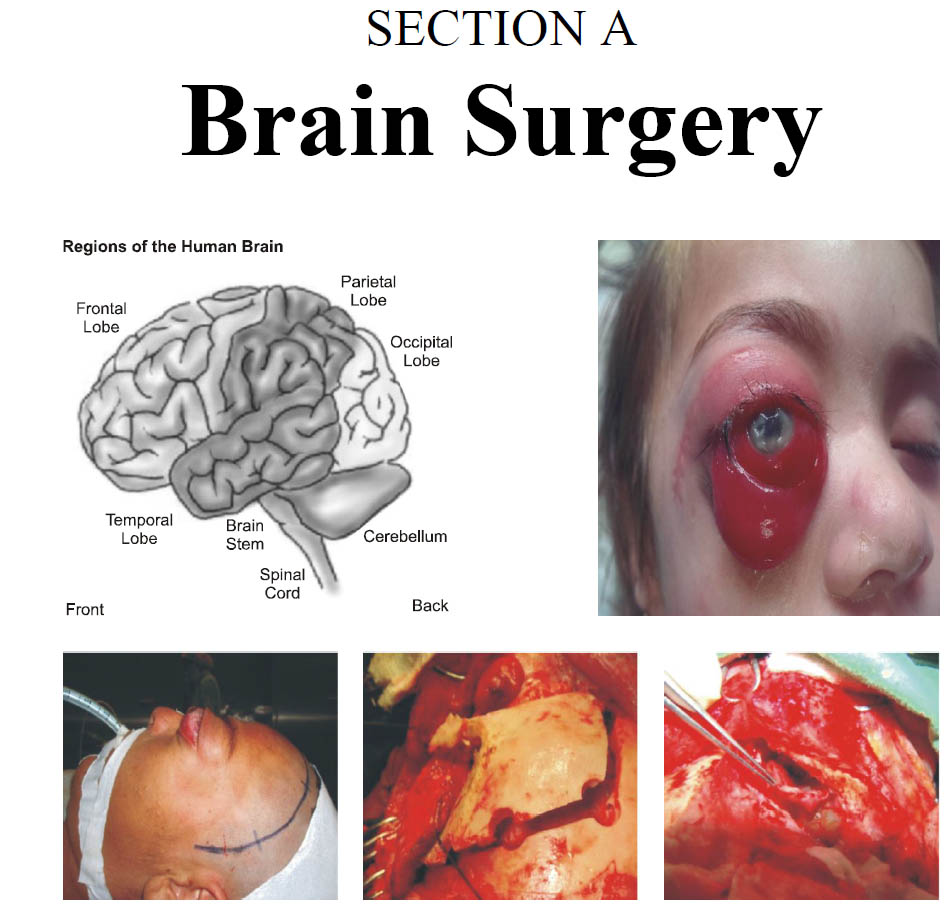
Results: We had 26 children in our study, age range about 1–3 years. Patients were cleaved into groups depending on their age. Most of the children 15 (57.6%) were in 1–2 years age group and 11 (42.3%) were in 2-3 years of age. Boys were 18 (69.2%) and girls were 8(30.7%). Coronal 11 (42.3%) was the most common suture involved, followed by sagittal 9 (34.6%). Lambdoid suture 3 (11.5%), metopic 2 (7.6%) and 3 (11.5%) case presented with raised intracranial pressure with multiple sutures closed involved. Strip craniectomy was done in all cases. We did bicoronal flap and Scalp flap turned into a supraorbital region while in metopic suture Fronto-orbital advancement and remodeling approach were used. No major complication was observed.
Conclusion: Cases which are managed early age have given good acceptable results in follow up, proper surgical expertise, perioperative management of temperature, blood loss, relieving the restriction of sutures and normalizing raised intracranial pressure can decrease the morbidity and mortality.
References
2. Cornelissen M, den Ottelander B, Rizopoulos D, van der Hulst R, van der Molen AM, van der Horst C, Delye H, van Veelen ML, Bonsel G, Mathijssen I. Increase of prevalence of craniosynostosis. Journal of Cranio-Maxillofacial Surgery. 2016; 44 (9): 1273-9.
3. Badve CA, Mallikarjunappa MK, Iyer RS, Ishak GE, Khanna PC. Craniosynostosis: imaging review and primer on computed tomography. Pediatric radiology.
2013; 43 (6): 728-42.
4. Wilkie AO, Johnson D, Wall SA. Clinical genetics of craniosynostosis. Current opinion in pediatrics. 2017; 29 (6): 622.
5. Massimi L, Bianchi F, Frassanito P, Calandrelli R, Tamburrini G, Caldarelli M. Imaging in craniosynostosis: when and what? Child's Nervous System. 2019; 9: 1-5.
6. Kutkowska-Ka?mierczak A, Gos M, Obersztyn E. Craniosynostosis as a clinical and diagnostic problem: molecular pathology and genetic counseling. Journal of applied genetics. 2018; 59 (2): 133-47.
7. Birgfeld CB, Dufton L, Naumann H, Hopper RA, Gruss JS, Haberkern CM, Speltz ML. Safety of Open Cranial Vault Surgery for Single Suture Craniosynostosis: A Case for the Multi-disciplinary Team. The Journal of craniofacial surgery. 2015; 26 (7): 2052.
8. Governale LS. Craniosynostosis. Pediatric neurology. 2015; 53 (5): 394-401.
9. Abraham P, Brandel MG, Dalle Ore CL, Reid CM, Kpaduwa CS, Lance S, Meltzer HS, Gosman AA. Predictors of postoperative complications of craniosynostosis repair in the national inpatient sample. Annals of plastic surgery. 2018; 80 (5S): S261-6.
10. Synèse BJ, Francis RW, Tony AR, Willy R, Mamiarisoa R, Clément A. Epidemiologic and surgical approach of cranyosynostosis: case of Madagascar and review of literature. Journal of Advance Research in Medical & Health Science (ISSN: 2208-2425). 2019; 5 (9): 01-13.
11. Haq EU, Aslam A, Kazmi A, Tammimy MS, Aman S, Ahmad RS. Fronto-orbital advancement and total calvarial remodelling for craniosynostosis. Journal of the College of Physicians and Surgeons Pakistan, 2014; 24 (2): 118-22.
12. Lionel KR, Natarajan A, Mariappan R, Singh G, Moorthy RK. A0018 Anesthetic Management of Children with Craniosynostosis for Corrective Surgery: A 10-Year Experience. Journal of Neuroanaesthesiology and Critical Care. 2019; 6 (01): A0018.
13. Sharma RK. Craniosynostosis in an Indian Scenario: A Long-term Follow-up. Plastic and Reconstructive Surgery–Global Open. 2020; 8 (3): e2696.
14. Shim KW, Park EK, Kim JS, Kim YO, Kim DS. Neurodevelopmental problems in non-syndromic craniosynostosis. Journal of Korean Neurosurgical Society. 2016; 59 (3): 242.
15. Lam S, Fridley J, Desai VR, Srinivasan VM, Jea A, Luerssen TG, Pan IW. Pediatric national surgical quality improvement program: useful for quality improvement in craniosynostosis surgery? Journal of Craniofacial Surgery. 2016; 27 (3): 605-11.
Downloads
Published
Issue
Section
License
The work published by PJNS is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Copyrights on any open access article published by Pakistan Journal of Neurological Surgery are retained by the author(s).












