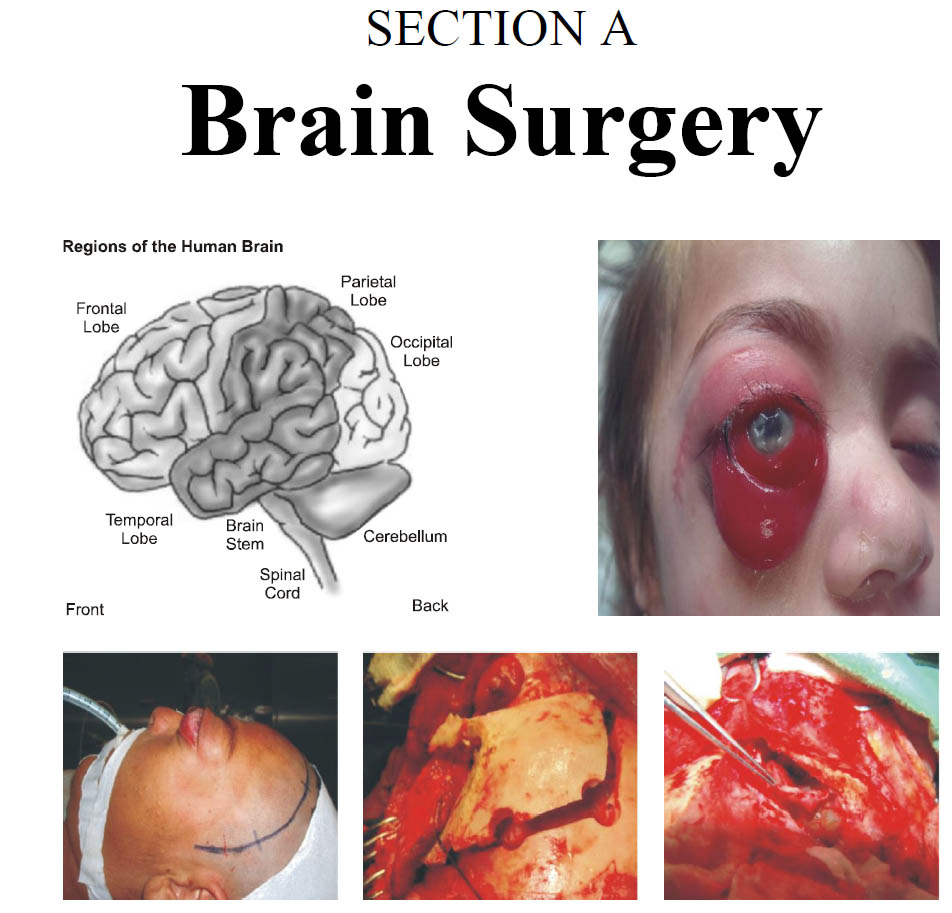
Microsurgical Resection of Intracranial Dermoid and Epidermoid Tumors
DOI:
https://doi.org/10.36552/pjns.v24i1.413Keywords:
Intracranial dermoid and epidermoid tumor, microsurgical resection of tumorAbstract
Objective: To Ascertain the outcome of microsurgical resection of intracranial dermoid and epidermoid tumors.
Materials and Methods: This prospective study was carried out in Neurosurgical Department, Lady Reading Hospital (LRH) Peshawar and followed for 3 years after microsurgical resection. All the patients with suspected intracranial Dermoid and epidermoid tumors (IDETs) on imaging study pre-operatively and later confirmed
postoperatively (after histopathology) were enrolled. Patients having recurrent tumor, opting for nonsurgical management and those deem unfit for surgery were not included in the study.
Results: 27 patients were included in the study with 12 (44.4%) males and 15 (56.6%) female. Age of the patients rangefrom 11 to 58 years.Mean age was 38.6 years. Epidermoid tumors were 19 (70.3%) in number and dermoid 8 (29.7%) in number. The most common presentation was increased intracranial pressure (ICP) and cranial
nerve deficit. The lesion was located in infratentorial location in 15 (56.6%) patients, 12(44.4%) were supratentorialy located. Gross total removal (GTR) was performed in 21 (77.8%) patients, while in six patients (22.2%) subtotal removal (STR) was attempted. 1 (3.7%) patient died while 2 (7.4%) patients had permanent morbidity post operatively, all other patients (89%) improved. Recurrence occurred in 9.5% of GTR patients while in STR patients, 33.3% patients were noted with increase in residual tumor on neuroimaging.
Conclusion: Microsurgical resection with GTR is possible for most IDET and gives good results with minimalcomplications.
References
2. Linkov G, Kanev PM, Isaacson G. Conservative management of typical pediatric postauriculardermoid cysts. Int J Pediatr Otorhinolaryngol. 2015; 79 (11):
1810–1813.
3. Zimny A, Zin?ska L, Bladowska J, Neska-Matuszewska M, Sasiadek M.Intracranial lesions with high signal intensity on T1-weighted MR images – review of pathologies. Pol J Radiol. 2013; 78 (04): 36–46.
Downloads
Published
Issue
Section
License
Copyright (c) 2020 AKRAM ULLAH, MUSAWER KHAN, MUMTAZ ALIThe work published by PJNS is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Copyrights on any open access article published by Pakistan Journal of Neurological Surgery are retained by the author(s).












