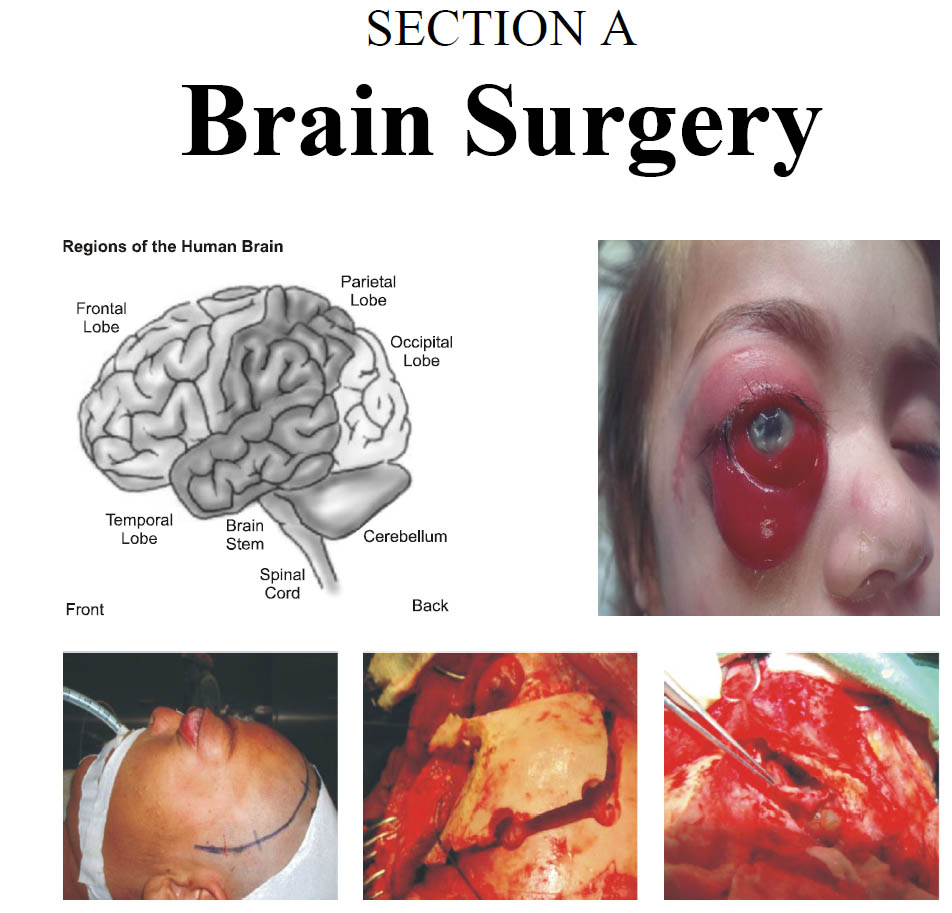
5 Years Mortality of Severe Traumatic Brain Injury during the Establishment of Closed System Neurocritical Care Unit in a Resource Constrained Developing Country
DOI:
https://doi.org/10.36552/pjns.v24i1.416Keywords:
Severe Traumatic Brain Injury, Standard Operating Protocols, Neurocritical CareAbstract
Background & Objectives: Severe traumatic brain injury is one of the leading causes of mortality and morbidity.Efficient management of severe traumatic brain injury demands a specialty driven focused intensive care. We developed our model of closed ICU driven by Neurosurgical Neurointensivist and the corollary to this
commitment is a TBI patient centered Neurocritical care with the capacity and capability to deal with most of the neurological illnesses.
Materials & Methods: A prospective study was conducted to find out the impact of the establishment of closed system of neurocritical care on 5 year mortality of severe TBI. Total 1288 patients met the inclusion criteria, which were enrolled. Tabulation was done for gender, age range, Glasgow outcome scale and mortality.
Results: It was observed that mortality reduced from 47% to 35% over a span of five years. The most common age range was 30-40 years, which is the most productive group of any population. Bed sore incidence is always on rise in any ICU. After the implementation of SOPs based management and increase in nursing staff the
incidence of bedsore also showed a detrimental pattern from 35 % to 19%.
Conclusion: Neurocritical care unit is proven to be an integral part of any neurosurgical unit and this closed system of NCC unit provide best SOP based care with significant reduction in mortality of patients with STBI.
References
2. McCredie VA, Alali AS, Scales DC, et al. Impact of ICU Structure and Processes of Care on Outcomes after Severe Traumatic Brain Injury: A Multicenter CohortStudy. Critical Care Medicine, 2018; 46 (7): 1139- 1149. DOI: 10.1097/ccm.0000000000003149.
3. Opondo EA, Mwangombe NJM. Outcome of severe traumatic brain injury at a critical care unit: a review of 87 patients. The Annals of African Surgery, 2005; 1: 3-9.
4. Tobi KU, Azeez AL, Agbedia SO. Outcome of traumatic brain injury in the intensive care unit: a five year review. South African Journal of Anaesthesia and Analgesia, 2016; 22: 5, 135-139.
Downloads
Published
Issue
Section
License
Copyright (c) 2020 SYED SHAHZAD HUSSAIN, USMAN AHAMD KAMBOH, ASIF RAZA, HUSNAIN TAHIR, RABIA RAZZAQ, MOHAMMED ASHRAF, NAVEED ASHRAFThe work published by PJNS is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Copyrights on any open access article published by Pakistan Journal of Neurological Surgery are retained by the author(s).












