Pattern of Presentation of Spinal Dysraphism: A Study of 72 Patients in Hayatabad Medical Complex Peshawar, Pakistan
DOI:
https://doi.org/10.36552/pjns.v24i3.433Keywords:
Spina bifida, myelomeningocele, spinal dysraphism.Abstract
Objective: To review the pattern of presentation and current understanding of patients with spinal dysraphism in our local population.
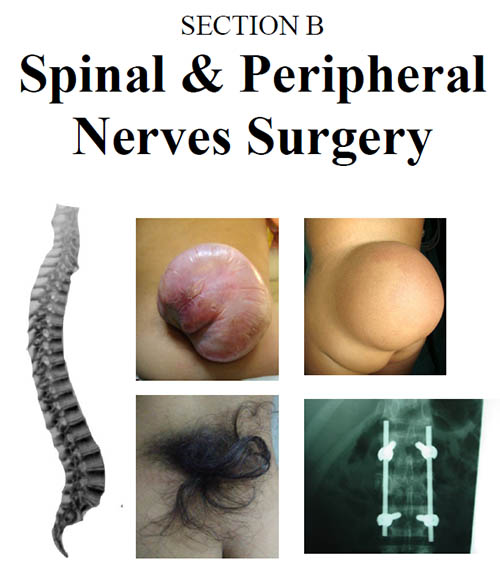
Material and Methods: Cases of spinal dysraphism of any gender and age were admitted via OPD, emergency or referred from another department were included in the study. Information on demographics, developmental history, presenting symptoms , presence/absence of back swelling, hairy patches, a nevus, dimple, an appendage/ skin tag, lower limb function, sensory/ motor deficit, bowel and bladder dysfunction were recorded. MRI spine was done in all patients to know the exact diagnosis.
Results: Out of 72 cases, 52 (72.2%) presented with spina bifida Aperta (spina bifida cystica) while 20 (27.7%) with spina bifida occulta. Total 53 (73.6%) patients presented at the age of 0 – 1 years. 41 (56.9%) of the patient presented with visible sac, 35 (48.6%) swelling over the back, in 5 (6.9%) of patient have hairy patch and dermal sinus each, while 28 (38.8%) patients have neurological deficit. Most common type of spinal dysraphism was myelomeningocele 45 (62.5%). Postoperative course of patients with spinal dysraphism was found to be uneventful in 56 (77.7%), wound infection was seen in 11 (15.2%), deterioration of neurological status in 3 (4.16%) of cases.
Conclusion: Spinal dysraphism is not an uncommon condition in our local population its clinical presentation and features are in line with internationally reported literature. Our population is least aware of the adverse neurological outcomes of the condition and face difficulties to access the adequate healthcare for spinal dysraphism.
References
2. Dawoud MF. Role of MRI in diagnosis of spinal congenital anomalies radiology and neurosurgery. Tanta Medical Sciences Journal 2007;2(1):182-193.
3. Kumar R, Singh SN. Spinal dysraphism: Trends in northern india Journal 2003;38(3):133-145
4. Shin M. Birth defects epidemiology and surveillance. Prevelance of spina bifida among children and adolescents in 10 regions in the united states. Jornal of Pediatrics 2010;126(2):174-9.
5. Rufener S, Ibrahim M, Parmar HA. Imaging of congenital spine and spinal cord malformations. Neuroimaging clin N Am 2011;21(3):59-76
6. Smith JL. Management of neural tube defects, hydrocephalus,refractory epilepsy and central nervous system infections. Pediatric surgery 2012; 12(1):1673-97.
7. Steinbok P.Dysraphic lesion of cervical spinal cord. Neurosurg clin N Am 1995; 69(2):367-76.
8. Boyd PA, Wallesley DG,De Walle HE,Tenconi R,Gracica-Minaur S,Zandwijkern GR, et al. Evaluation of the prenatal diagnosis of neural tube defect by fetal ultasonographic examination in different centre across Europe. Journal of Medical Screen 2000;7(1):169-74.
9. Dias MS, Partington M. Embryology of myelomeningocele and anencephaly. Neurosurg Focus 2004;16(2):174-79.
10. Hashim AS, Ahmed S, Jooma R. Management of meyelomeningocele. Journal of surgery(international) 2008;13(1):
11. Johnson MP, Grades M, Rintoul N,Pasquariello P, Melchionni J,Sutton N et al. Maternal-fetal surgery for myelomeningocele:Neurodevelopmentat outcome at 2 years of age. Am Journal Obstret Gynecol 2006;194(3):1145-50.
12. Kumari MV,Suprya P, Aemjal SC, et al. Role of MRI in evaluation of suspected spinal dysraphism. J. Evolution Med.Dent.Sci. 2016;5(17):879-884.
13. Copp AJ, Stanier P, Greene NDE. Neural tube defect-recent advances unsolved question and controversies. Lancet Neurology 2013;12(8):799-810.
14. Nishtar T, Elahi A, Iqbal N. To determine the frequency of accuracy of MRI in diagnosis of rare disorder of spinal dysraphism. J Med Sci 2011;19(4):195-199.
15. Ackermal LL, Menezes AH. Spinal congenital dermal sinuss:A 30 years experience. Journal of Pediatric 2003;112(5):641-647.
16. Kumar R, Singh SN. Spinal dysraphism: Trends in northern india Journal 2003;38(3):133-145
17. Venkatesh KL. Study of clinical profile and associated anomalies and surgical outcome of spina bifida. Int Surg J 2017;4:141-5.
18. Pornswan Wasant, Achara Sathienkijkanchai. Neural tube defects at Siriraj Hospital Bangkok-10years review. J Med Assoc Thai 2005;88(8):115-119.
19. Ahmed M, Limbu CP,Mughal SH. Pattern of presentation of spinal dysraphism. Pak J of Neurol Surg. 2010;14(2):127-130.
20. Asindi Asindi, Ameer AL. Neural tube defect in the Asir region of Saudi Arabia. Annal of Saudi Mediciene 2001;21(1):169-74.
21. Galhom AE, Deeb WA, Osama A. Early clinical characteristics and surgical outcome in 10 children with occult spinal dysraphism. Egypt J Neurol Psychiat Neurosurg 2013;50(2):127-34.
22. Erfani MA, Ganjavian MS, Ameri E, Namazi H, Sooloki S, Samini M. Orthopedic lesion in tethered cord syndrome: the importance of early diagnosis and treatment on patient outcome.Arch Bone Joint Surg. 2014;292):53-57
Downloads
Published
Issue
Section
License
The work published by PJNS is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Copyrights on any open access article published by Pakistan Journal of Neurological Surgery are retained by the author(s).












