Surgical Outcome of Sellar Suprasellar Brain Tumors through Retracterless Subfrontal Approach
DOI:
https://doi.org/10.36552/pjns.v25i1.530Keywords:
Sellar and Suprasellar brain tumors, Retractorless Method,, Subfrontal ApproachAbstract
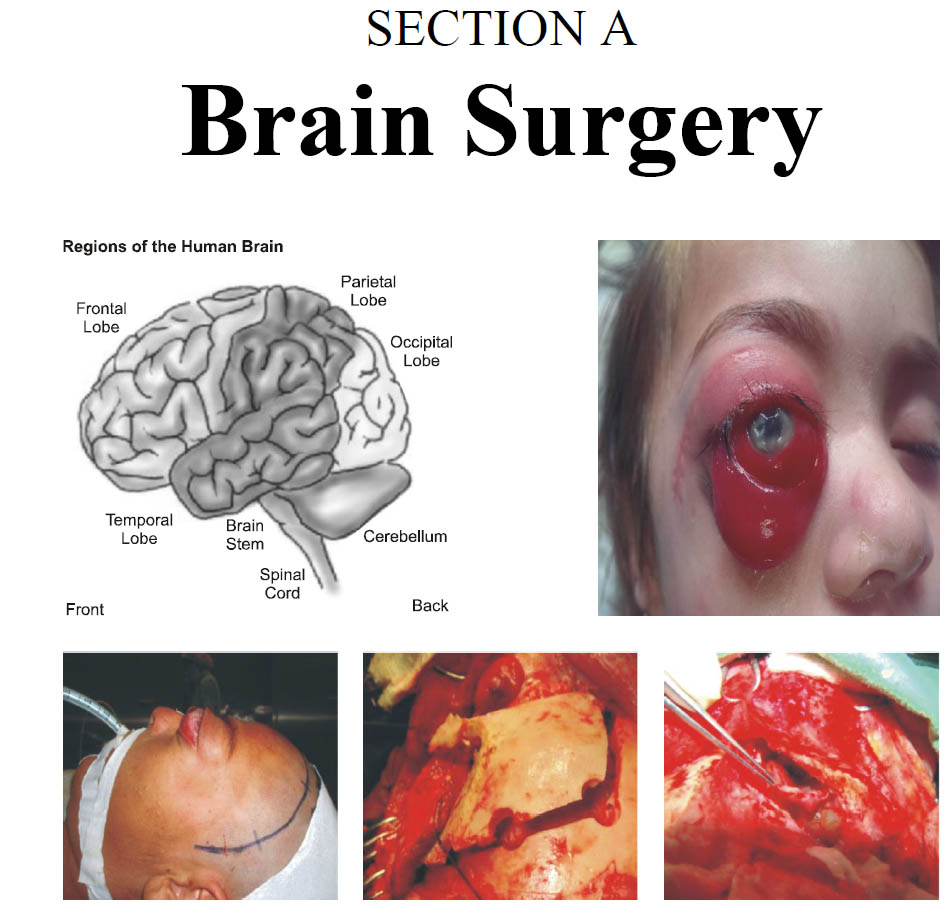
Objectives: The aim of this study is to see the surgical outcome of Sellar and Suprasellar brain tumors with retractorless modified subfrontal approach.
Material and Methods: We did cohort study of 15 patients who were operated in Neurosurgery Unit 2, PINS. Our study duration is 1 year and follow up duration is of 3 months. Clinical features were related to cranial nerves 2nd, 3rd ,4th, and pituitary gland, dural irritation and temporal lobe compression i.e., diplopia, decrease vision, CSF rhinorrhea, abnormal olfaction, headache, GTCS etc.
Results: In our study, age range was 8 – 62 years with mean age was 35 years. Our 5 patients were male and 10 patients were female. Surgery was performed in all patients through subfrontal approach with retractorless method. In Histopathological report of 2 patients’ findings was Craniopharyngioma, 12 were of pituitary adenoma and 1 was of sellar meningioma. Seven 46.67 percent patients operated successfully with no new neurological deficit. Three 20 percent patients operated but no post op improvement in clinical symptoms, no patients were re-explored postoperatively due to CSF Rhinorrhea. Diabetes Insipidus occurred in 5 (33.3%) patients post-operatively which was managed later on.
Conclusion: Surgery subfrontal approach with retractorless method is the safe corridor for treatment of sellar and Suprasellar brain tumors.
References
2. Patel H, Tiwari V. Stat Pearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Oct 27, 2018. Physiology, Posterior Pituitary.
3. Shahid Z, Singh G. Stat Pearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Dec 9, 2018. Physiology, Hypothalamus.
4. Monson JP. The epidemiology of endocrine tumours. Endocrine-related cancer, 2000 Mar 1; 7 (1): 29-36.
5. Al-Shraim M, Asa SL. The 2004 World Health Organization classification of pituitary tumors: what is new? Acta Neuropathologica. 2006 Jan; 111 (1): 1-7.
6. Asa SL, Kovacs K. Clinically non-functioning human pituitary adenomas. Canadian Journal of Neurological Sciences, 1992; 19 (2): 228-35.
7. Snyder PJ. Clinically nonfunctioning pituitary adenomas. Endocrinology and metabolism clinics of North America. 1993; 22 (1): 163-75.
8. Greenman Y, Melmed S. Diagnosis and management of nonfunctioning pituitary tumors. Annu Rev Med. 1996; 47: 95-106.
9. Flickinger JC, Nelson PB, Maninez AJ, et al. Radiotherapy of nonfunctional adenomas of the pituitary gland. Results with long term follow-up. Cancer, 1989; 63: 2409-2414.
10. Greenman Y, Mclmed S. Diagnosis and management of nonfunctioning pituitary tumors. Annu Rev Med. 1996; 47: 95-106.
14. Elster AD. Imaging of the sella: anatomy and pathology. In Seminars in Ultrasound, CT and MRI, 1993 Jun 1; Vol. 14, No. 3: pp. 182-194. WB Saunders.
15. Chiang MF, Brock M, Patt S. Pituitary metastases. Neurochirurgia. 1990; 33 (04): 127-31.
16. Mortini P, Losa M, Barzaghi R, Boari N, Giovanelli M. Results of transsphenoidal surgery in a large series of patients with pituitary adenoma. Neurosurgery, 2005; 56 (6): 1222-33.
17. Alleyne CHJ, Barrow DL, Oyesiku NM. Combined transsphenoidal and pterional craniotomy approach to giant pituitary tumors. Surg Neuro. 2002; 57: 380-390.
18. Ragel BT, Couldwell WT. Pituitary carcinoma: a review of the literature. Neurosurgical focus, 2004 Apr. 1; 16 (4): 1-9.
19. Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery, 1993; 33 (4): 610-8.
20. Powell M. Recovery of vision following transsphenoidal surgery for pituitary adenomas. British Journal of Neurosurgery, 1995; 9 (3): 367-74.
21. De Menis E, VISentin A, Billeci D, et al. Pituitary adenomas in childhood and adolescence. Clinical analysis of 10 cases. Endocrinol Invest. 2001; 24 (2): 92-97.
22. Artese R, D'Osvaldo DH, Molocznik I, Benencia H, Oviedo J, Burdman JA, Basso A. Pituitary tumors in adolescent patients. Neurological Research, 1998; 20 (5): 415-7.
23. Ikram MF, Sajjad Z, Shokh IS, Omair A. Pituitary gland volume on magnetic resonance imaging: Normative observations. Pak J Neurol Sci. 2007; 2: 141-4.
Downloads
Published
Issue
Section
License
The work published by PJNS is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Copyrights on any open access article published by Pakistan Journal of Neurological Surgery are retained by the author(s).












